Medical Device Needs in Diabetic Patients for Achieving Diabetes Remission: A Case Study of Ban Ta Khun District, Surat Thani Province
Keywords:
Medical Device Needs, Diabetic Patients, Digital Health, Diabetes RemissionAbstract
This qualitative research aimed to explore the needs for medical device utilization to achieve diabetes remission among patients with diabetes in Ban Ta Khun District, Surat Thani Province. A total of 15 key informants participated in the study, including five individuals diagnosed with type 2 diabetes, four family caregivers, one physician from the diabetes clinic, three nurses, one nutritionist, and one IT system officer. Data collection tools included in-depth interviews, observations, field notes, and audio recordings. The data were analyzed using content analysis.
An external quality review was conducted by three experts in diabetes care to confirm the consistency and appropriateness of the research. The findings revealed that
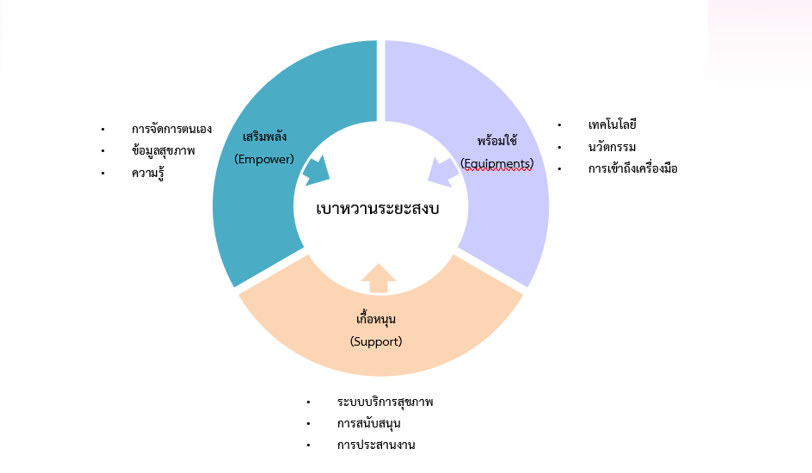
The informants expressed needs for medical devices to achieve diabetes remission, which could be categorized into three main themes 1) Empowerment, which comprised three subthemes: self-management, health information, and knowledge; 2) Accessible and ready-to-use tools, consisting of technology, innovation, and accessibility of medical devices; and 3) Support systems, with subthemes of healthcare system support, professional support, and coordination. The results reflect a paradigm shift from viewing patients as passive recipients of care to recognizing them as proactive partners in managing their own health. These needs highlight that medical devices, in the context of achieving diabetes remission, are not merely tools for measurement and recording. Rather, they serve as critical instruments for empowerment—enhancing patients’ capabilities, confidence, and motivation to manage their condition effectively. This requires a supportive healthcare system that facilitates access and the use of appropriate technology.
Future research should explore the development of digital support systems and integrated services that bridge gaps in accessibility and enhance the skills required for sustainable use of medical devices among people with diabetes.
References
สมาคมเบาหวานแห่งประเทศไทย. (2566). แนวทางเวชปฏิบัติสำหรับโรคเบาหวาน ประจำปี 2566. กรุงเทพฯ: สมาคมเบาหวานแห่งประเทศไทย
Alcántara-Aragón V. (2019). Improving patient self-care using diabetes technologies. Ther Adv Endocrinol Metab. doi: 10.1177/2042018818824215.
Bandura, A. (1997). Self-efficacy: The exercise of control. New York: W.H. Freeman. Baig, A. A., Benitez, A., Quinn, M. T., & Burnet, D. L. (2015). Family interventions to improve diabetes outcomes for adults. Annals of the New York Academy of Sciences, 1353(1), 89–112. https://doi.org/10.1111/nyas.12844.
Creswell, J. W. (2018). Research design: Qualitative, quantitative, and mixed methods approaches (5th ed.). Thousand Oaks, CA: SAGE Publications.
Epstein, R. M., & Street, R. L. (2011). The values and value of patient-centered care. Annals of Family Medicine, 9(2), 100–103. https://doi.org/10.1370/afm.1239
Funnell, M. M., & Anderson, R. M. (2004). Empowerment and self-management of diabetes. Clinical Diabetes, 22(3), 123–127. https://doi.org/10.2337/diaclin.22.3.123
Fisher, E. B., Thorpe, C. T., DeVellis, B. M., & DeVellis, R. F. (2005). Healthy coping, negative emotions, and diabetes management: A systematic review and appraisal. The Diabetes Educator, 33(6), 1080–1103. https://doi.org/10.1177/0145721707309808.
Glasgow, R. E., Davis, C. L., Funnell, M. M., & Beck, A. (2001). Implementing practical interventions to support chronic illness self-management. Joint Commission Journal on Quality and Patient Safety, 27(11), 575–584.
Greenwood, D. A., Gee, P. M., Fatkin, K. J., & Peeples, M. (2017). A systematic review of reviews evaluating technology-enabled diabetes self-management education and support. Journal of Diabetes Science and Technology, 11(5), 1015–1027. https://doi.org/10.1177/1932296817713506
Hou, C., Xu, Q., Diao, S., & Hewitt, J. (2018). Mobile phone applications and self-management of diabetes: A systematic review with meta-analysis, meta-regression of 21 randomized trials. JMIR mHealth and uHealth, 6(12), e12297. https://doi.org/10.2196/12297
International Diabetes Federation. (2022). IDF Diabetes Atlas (10th ed.). Retrieved from https://diabetesatlas.org.
Lincoln, Y. S., & Guba, E. G. (1985). Naturalistic inquiry. Sage Publications.
Ouwens, M., Wollersheim, H., Hermens, R., Hulscher, M., & Grol, R. (2005). Integrated care programmes for chronically ill patients: A review of systematic reviews. International Journal for Quality in Health Care, 17(2), 141–146. https://doi.org/10.1093/intqhc/mzi016
Powers, M. A., Bardsley, J., Cypress, M., Duker, P., Funnell, M. M., Fischl, A. H., ... & Vivian, E. (2009). Diabetes self-management education and support in type 2 diabetes. The Diabetes Educator, 35(Suppl 3), 85S–107S. https://doi.org/10.1177/0145721709331946.
U.S. Department of Health and Human Services. (2022). Electronic health records and telehealth adoption increase to reduce hospital burden. Retrieved from https://www.hhs.gov.
UNICEF. (2022). Ireland harnesses health technology to reach 2.5 billion people, including elderly and persons with disabilities. Retrieved from https://www.unicef.org. World Health Organization. (2021). Diabetes. Retrieved from https://www.who.int/news-room/fact-sheets/detail/diabetes.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Nursing Innovation and Health Association Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.

