5-year recurrent rate and factors related recurrent spinal meningioma
Keywords:
Spinal meningioma, Recurrent meningioma, Recurrent rate, Recurrent factor, Spinal cord tumorAbstract
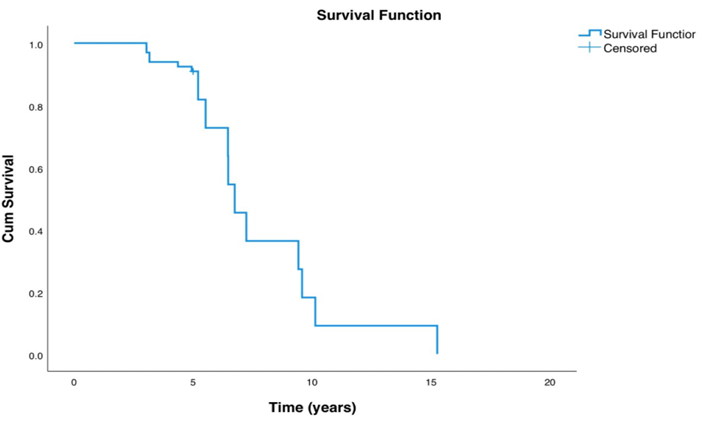
Introduction: Spinal meningiomas are usually benign spinal cord tumors, representing about 25% of all spinal tumors. Treatment options include watchful waiting and surgery, which typically removes the tumor completely with a low recurrence risk. However, undetected recurrences can cause neurological issues, necessitating regular MRI scans. Previous studies showed a 7-9% recurrence rate at 5 years post- surgery, increasing to 20-25% after 10 years3. This study aims to find 5-year recurrence rate and related factors for recurrence. Methods: The authors conducted a single-center retrospective descriptive study in patients with spinal meningiomas treated in Siriraj hospital from July 2006 to November 2024. Finding 5-year and overall recurrence rate of 66 spinal meningiomas and related factors for recurrence. Results: 5-year and overall recurrence rates were 10.6% and 24.2%, respectively. The factors mostly affected recurrence were younger age at diagnosis (esp. <45 years) and history of neurofibromatosis type 2 (NF2). Other factors included gender, volume, location of tumor, dural tail sign, histopathological diagnosis and intra-operative finding did not showed statistically significance for tumor recurrence. Conclusions: The study at Siriraj Hospital shows that surgical removal of spinal meningiomas is effective but has a significant risk of recurrence, especially in younger patients or those with NF2. Despite benign nature of disease, our findings emphasize the importance of careful surgery and long-term follow-up. High-risk groups may need early and more frequent investigation.
Downloads
References
Kshettry VR, Hsieh JK, Ostrom QT, Kruchko CB, Benzel EC, Barnholtz-Sloan JS. Descriptive epidemiology of spinal meningiomas in the United States. Spine. 2015;40(12):886-9. https://doi.org/10.1097/BRS.0000000000000974
Solero CL, Fornari M, Giombini S, Lasio G, Oliveri G, Cimino C, et al. Spinal meningiomas: review of 174 operated cases. Neurosurgery. 1989; 25(2):153-60. https://doi.org/10.1227/00006123-198908000 00001
Kwee LE, Harhangi BS, Ponne GA, Kros JM, Dirven CMF. Spinal meningiomas: treatment outcome and long-term follow-up. Clin Neurol Neurosurg. 2020;198:106238. https://doi.org/10.1016/j.clineuro.2020.106238
Tsuda K, Akutsu H, Yamamoto T, Nakai K, Ishika wa E, Matsumura A. Is Simpson grade I removal necessary in all cases of spinal meningioma? Assessment of postoperative recurrence during long-term follow-up. Neurol Med Chir (Tokyo). 2014;54(11):907-13. https://doi.org/10.2176/nmc.oa.20130311
Maiuri F, Di Divitiis O, Guadagno E, Mariniello G. Recurrence of spinal meningioma: analysis of the risk factors. Br J Neurosurg. 2020;34(5):569 74. https://doi.org/10.1080/02688697.2019.1638886
Wang ZL, Mou JH, Sun D, Liu P. Upper thoracic purely extradural spinal meningioma with nerve root attachment: a case report and literature review. Front Surg. 2022;9:918094. https://doi.org/10.3389/fsurg.2022.918094
Mirimanoff RO, Dosoretz DE, Linggood RM, Ojemann RG, Martuza RL. Meningioma: analysis of recurrence and progression following neuro surgical resection. J Neurosurg. 1985;62(1):18 24. https://doi.org/10.3171/jns.1985.62.1.0018
Cohen-Gadol AA, Zikel OM, Koch CA, Scheithauer BW, Krauss WE. Spinal meningiomas in patients younger than 50 years of age: a 21-year experience. J Neurosurg. 2003;98(3 Suppl): 258-63. https://doi.org/10.3171/spi.2003.98.3.0258
Deska-Gauthier D, Hachem LD, Wang JZ, Landry AP, Yefet L, Gui C, et al. Clinical, molecular, and genetic features of spinal meningiomas. Neu rooncol Adv. 2024;6(Suppl 3):iii73-82. https://doi.org/10.1093/noajnl/vdae123
Goutagny S, Kalamarides M. Meningiomas and neurofibromatosis. J Neurooncol. 2010; 99(3):341-7. https://doi.org/10.1007/s11060-010-0339-x
Kobayashi K, Ando K, Matsumoto T, Sato K, Kato F, Kanemura T, et al. Clinical features and prognostic factors in spinal meningioma surgery from a multicenter study. Sci Rep. 2021;11(1): 11630. https://doi.org/10.1038/s41598-021-91225-z
Gottfried ON, Gluf W, Quinones-Hinojosa A, Kan P, Schmidt MH. Spinal meningiomas: surgical management and outcome. Neurosurg Focus. 2003;14(6):e2. https://doi.org/10.3171/foc.2003.14.6.2
Maiti TK, Bir SC, Patra DP, Kalakoti P, Guthi konda B, Nanda A. Spinal meningiomas: clini coradiological factors predicting recurrence and functional outcome. Neurosurg Focus. 2016;41(2):E6. https://doi.org/10.3171/2016.5.FOCUS16163
Nakamura M, Tsuji O, Fujiyoshi K, Hosogane N, Watanabe K, Tsuji T, et al. Long-term surgical outcomes of spinal meningiomas. Spine (Phila Pa 1976). 2012;37(10):E617-23. https://doi.org/10.1097/BRS.0b013e31824167f1
Arima H, Takami T, Yamagata T, Tanaka S, Tsuyuguchi N, Ohata K. Surgical management of spinal meningiomas: a retrospective case analysis based on preoperative surgical grade. Surg Neurol Int. 2014;5(Suppl 7):S333-8. https://doi.org/10.4103/2152-7806.139642
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Thai Journal of Neurological Surgery

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Articles in this journal are copyrighted by the x may be read and used for academic purposes, such as teaching, research, or citation, with proper credit given to the author and the journal.use or modification of the articles is prohibited without permission.
statements expressed in the articles are solely the opinions of the authors.
authors are fully responsible for the content and accuracy of their articles.
other reuse or republication requires permission from the journal."


